Diarrhoea with Blood in Stools in Children
Ask a Question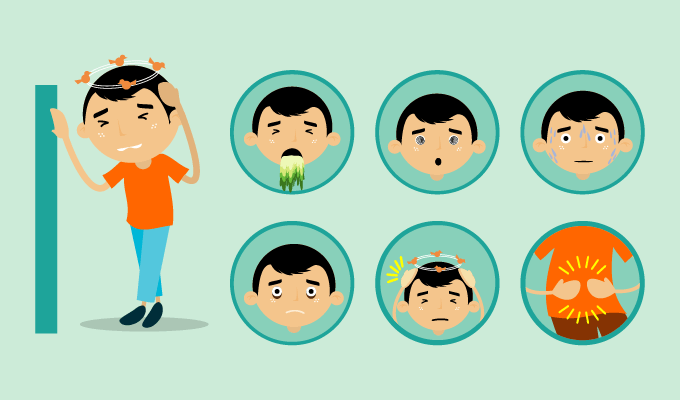
Children, especially in their school age, are susceptible to get abdominal pain or diarrhoea, commonly induced by bacterial infection. However, if there is blood in their stools, accompanied by fever, parents should raise the alert that whether the child gets ulcerative colitis. It’s better to see your doctors to determine the explicit disease and accept treatment immediately, in case of dehydration.
What is ulcerative colitis?
Ulcerative colitis (UC) in children refers to nonspecific chronic inflammation of the inner lining of the colon (large intestine). The inflammation, caused by unknown factors, always begins in the left colon and gradually extends to the entire colon or even to the end of the ileum. Male and female are equally affected, starting with their childhood and later in life. However, UC rarely attacks babies and often occurs in adolescents or schoolchildren.
1. Symptoms of UC
Common symptoms
If children with ulcerative colitis suffer from the recurrent ulcerative colitis or acute attacks, they may experience:
• Diarrhoea with blood in the stool
• Fever
• Abdominal pain
• Poor appetite
Most of them have pale features, anaemia, malnutrition and developmental delay because of the long-lasting symptoms mentioned above.
Other symptoms that occur through the intestines:
• Some sufferers accompany diarrhoea with arthritis in limbs and spine
• 10% of patients have skin lesions like Erythema nodosum and Pyoderma gangrenosum.
• 2% of children with common symptoms suffer from retinitis and oral ulcers.
2. Laboratory tests. Bowel movements and stool culture, barium enema and colonoscopy.
3. The diagnosis is based on the clinical manifestation, medical history and the result of laboratory tests.
4. Complication: Fulminant ulcerative colitis, toxic megacolon, intestinal perforation, polyps, and cancer can occur in severe cases where the colon is completely infected. Although there are few cases of cancer in children, they should undergo a colonoscopy each year as the risk of cancer increases due to the prolonged course of the disease.
What are the causes of ulcerative colitis in children?
To date, the explicit cause of ulcerative colitis in children is hard to be defined by modern medicine. However, scientists found that UC is caused by the pathological lesion of inflammation of the inner wall of the colon in the form of ulcers or erosion. And the current consensus is that the immune factor, the genetic factor, and other factors can trigger the UC.
1. Autoimmune factor
Patients with ulcerative colitis always have one or more immunologic deficiency diseases such as AIH (autoimmune hemolytic), RA (rheumatoid arthritis), lupus and iris, which can be treated by adrenal hormones or other immunosuppressive therapies. Therefore, UC could be considered as a type of immune disorder.
2. Infection factor
Infection is the main trigger for the US. If the symptoms can be controlled or treated with antibiotics while UC is attacking, it may indicate that UC is closely related to the infection.
3. Food allergy
Some children are allergic to foods such as milk. When dairy products are removed from the diet, the obvious therapeutic effect may occur.
4. Genetic factor
About 30% to 50% of patients have a family history.
5. Emotional factor
In many clinical cases of UC in children, the symptoms may be accompanied by autonomic dysfunctions like anxiety, tension, and suspicion, which can be alleviated by psychotherapy.
From the perspective of eastern medicine, ulcerative colitis is triggered by:
1. Pathogenesis factor:
The external pathogens, which can cause diarrhoea, often attack the body in the form of heat, dampness, cold and fever. In particular, dampness can disturb the normal activities of the spleen. As soon as the patients eat the grain mixed with water, they will suffer from diarrhoea.
2. Excessive eating and drinking
Excessive eating and drinking can contribute to the burden of the stomach and form a stasis that is hard to digest. Otherwise, if you have a dampness-heat stomach and intestines, eating fatty and sweet foods can increase the risk of UC.
3. Unbalanced diet or illness
Weak spleen and stomach with unbalanced diet for a long time. Prolonged illness and tiredness can damage the spleen and the stomach.
4. Kidney-yang deficiency. The weak kidney in the absence of yang can affect the absorptive capacity of the stomach, leading to diarrhoea, so patients should limit the intake of water to prevent yin from increasing.
How to treat ulcerative colitis in children?
1. Non-surgical therapy
Non-surgical therapy with dietary therapy and drug therapy helps to relieve the symptoms and improve the nutritional status.
Dietary therapy
For children with ulcerative colitis, maintaining nutrition and eliminating the disruption of water-electrolytes can help relieve anaemia and hypoproteinemia.
• During flare-ups, the absolute diet offers the intestine a chance for recovery. When the symptoms subside, you can start with the vegetarian diet.
• During the intermission, it’s beneficial for patients to take digestible food that is low in fibre, rich in proteins and carbohydrates.
Drug therapy
• Sulfonamides are suitable for the patient with mild or moderate degree.
• Metronidazole can effectively reduce the symptom of tenesmus (ineffective, painful urge to move one's bowels caused by the inflammation) especially for the patient with anus disease.
• Antibiotics such as penicillin may also reduce the symptoms of tenesmus and should be taken by children with secondary inflammation of UC.
2. Surgery therapy
When is surgery recommended?
• Children whose symptoms are not alleviated after many years of symptomatic treatment.
• When it seriously affects children's growth and development.
• When some indications such as colonic stenosis, colonic perforation, massive hemorrhage, and toxic megacolon occur during symptomatic treatment.
Surgery for ulcerative colitis
The surgical method should be based on the age of the child, the course of the disease and extent of the symptoms. Here are examples of surgical methods:
• Subtotal Colectomy
• Total colectomy
• Permanent intestinal stoma
How to prevent ulcerative colitis?
• So far, there are no explicit precautions, but it seems plausible that a sensible diet and good eating habits are beneficial to stay healthy.
• To get rid of inflammation in the digestive system, try to strengthening exercises, avoid excessive tension, improve your diet and promote physical and mental health.
• Regular examination helps to diagnose and treat UC early.
• Subsequent visits are necessary to prevent the disease deteriorating.
Share: